Dental Implants- A Comprehensive Review
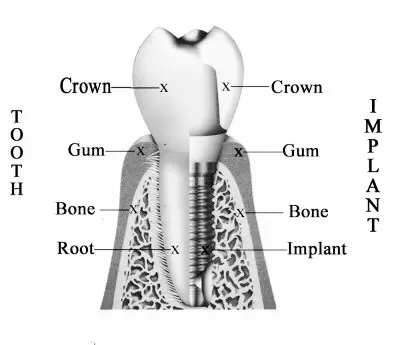
Dental implants as they are known today were introduced back in the year 1952 by a Swedish orthopedic surgeon known as Per-Ingvar Brånemark. Today dental implants are considered as the standard of care for replacement of a missing tooth or teeth. A dental implant is defined as a surgical fixture that is placed into the jawbone and allowed to fuse with the jaw bone over a span of a few month. The process by which dental implants fuses with the jaw bone is referred to as Osseointegration. Dental implant uses an artificial tooth that is usually made of titanium or other ceramic material. Titanium is the most preferred material for a dental implant since the body does not recognize it as a foreign object. The artificial tooth root that has been placed serves to hold a replacement bridge, crown, denture, facial prosthesis or acts as an orthodontic anchor. Having a dental implant fused into the jaw bone is the closest thing ever made to mimicking real natural teeth because the tooth stands on its own without affecting any of its neighbouring teeth and also has great stability. Technology in the field of dental implants has advanced in a great way to the extent that the success rate of dental implants today is almost a hundred percent.
During a dental implant process, the oral surgeon surgically places the titanium implant in the jaw with the top of the implant slightly above the top of the bone. The screw inserted is then sealed at the top so as to prevent any debris and other materials from getting into the implant. After that, the implant is given some few months, normally six months to allow it to Osseointegrate with the jaw bone. Dental implants can be used to replace a single, several, or even all the teeth in the mouth. The main goal is to restore the normal functioning of the teeth as well as aesthetic.
Dental implants failure are very rare. The success rate is between 95 to 98%. However, there is that small chance that a failure can occur during a dental implant process. There are various factor that can lead to dental implant failure. They include microbiological or biological factors, biomaterial factors, biomechanical factors or due to implant surface treatments. The most common cause of dental implant failure is due to poor oral hygiene. The build-up of debris and dental plaque around the implants results in an increase of bacterial infection. The practice of good oral hygiene can reduce this significantly. Another main reason for dental failure is an improper selection of an implant candidate. The health of the patient and the health of the tissues in the mouth also plays an integral role when it comes to success or failure of a dental implant. The planning stage is very essential when it comes to the evaluation of a patient. The dentist evaluates the amount of stress that will be subjected on the fixture and implant during normal function. Additionally, planning the position and number of implants to be placed is important since it can affect the long-term health of the prosthetic since the biomechanical forces that are created during chewing can be significant. The position by which the oral surgeon will place the implant is by great extent determined by the angle and position of the adjacent teeth by using computed tomography with Cast-based guided surgical guide (CAD) and computer-assisted design and manufacturing (CAM). After the surgery, the patient in most cases will experience some pain and minor discomforts, so the dentist will prescribe some pain medications so as to ease the discomfort. The patient is also advised to take soft foods, cold foods, and some warm soup.
When it comes to tooth replacement, the patient has two methods to choose from. The first option is removable dental appliance where the patient can be able to remove it from the mouth. The other option is a fixed or permanent dental appliance where once the dentist installs it, the patient cannot be able to remove it. Deciding which option to choose depends on a number of factors. Such factors include the health of the patient, the location of the missing tooth or teeth, and quality and quantity of the jaw bone where the dental implant is to be placed. Other factors include the cost of the dental implant and the patient preference. Some implants require a second surgery but if the dentist verifies that it is healed and okay, tooth replacement can now be fixed. The denture, crown or bridge will either be fixed using dental cement or lag screws.
With any medical surgery, there are always some risks associated with it, and dental implants surgery is no exemption. Careful planning of the dental implant surgery is important so as to mitigate the risk. It is important to make sure that the patient is healthy enough to go through the process. The risk and complications associated with dental implants are divided in three. There those risk and complications that occur during the surgery such as nerve injury or excessive bleeding and there are those that can occur within the first six months such as failure to Osseointegrate and infections. There are also those that can occur in the long term such as mechanical failures. Fortunately, the success rate of this process is high, and failures only occur in an unfortunate event of infections, overloading of dental implants, poor bone quality and quantity, damage of the surrounding area (blood vessels, nerve, and teeth) and fracture of the dental implant. Careful planning with a well-trained and qualified dental surgeon can help avoid all these risks. Dentist at Carrum Downs are well-trained and has years of experience dealing with dental implant treatment.
Contents
- Medical Uses
- Planning
- Healing Time
- Additional Surgical Procedure
- Bone Grafting
- Soft Tissue (Gingiva) Reconstruction
- Maintenance
- Risk and Complications
- Implant Failure
- Reduce Risk for Failure
Medical Uses
Dental implants are often the best choice when it comes to tooth replacement compared to all other tooth replacement options. There are stable and strong. A dental implant restores a lost tooth so that it can look, feel and function just as natural tooth. Other replacement options can lead to deterioration of the bone and may interfere with speaking, smiling, eating and other day to day activities. The main reason of having dental implants is to support dental prosthetics. Dental implants today make use of Osseointegration. The integration can last for a lifetime supporting physical loads when properly taken care of. For a single tooth replacement, first, an implant abutment is secured to the implant using a screw. Then a crown is attached to the abutment using dental cement, fused with the abutment as one piece during fabrication or through a small screw. Also, dental implants are used to retain a multiple tooth dental prosthesis either inform of removable dentures or fixed bridge.
With dental implants, there is no need to feel uncomfortable in public or stay at home, embarrassed because one feels like his/her smile looks different from others. A patient should also not feel uncomfortable that his/her teeth might fall out while speaking. Dental implants are very stable, and none of these occurrences can happen. Dental implants also restore a natural face of a patient. A face without teeth can appear to sag or sunken and sad. Dental implants allow a patient to maintain the natural face shape. As discussed earlier a fixed denture also known as an implant-supported bridge is a group of teeth that have been secured to dental implants in a way that the user cannot remove the prosthetic. Normally, bridges can connect to more than one implant and may also connect to teeth as anchor points. Typically, the number of teeth will be more than the anchor points with the teeth that are directly below the anchor points referred to as abutments and those that are not below the anchor points referred to as pontics. A fixed bridge can be used to replace two teeth and may even extend to the entire mouth.
Planning
Planning for a dental implant is probably the most important step in the entire dental implant treatment. Depending on the complexity of the case, a various number of oral practitioners may be involved in this particular stage. The oral surgeon is the doctor who will be involved in the placement of the implants inside the jawbone and perform all the other additional surgical, dental procedures. A prosthodontist is the physician who is in charge of prosthetic phase and the planning of a particular type of prosthesis. Gnathologist is a medical specialist who creates a functional occlusion in order to evenly distribute the chewing forces across the prosthetics the implants support. Other specialists that may be involved include dental technician and physicians of other specialties. In less complex cases one or two specialists mentioned can be able to handle the procedure properly. Advancement of technology has also enabled dental practitioners to be able to use computer developed software to plan for a dental implant accurately.
During the planning stage, there are some important considerations that the dental practitioner must put in place. Some of them include the data obtained from the physician examination and medical history and information gathered from the CT scan, dental x-rays, and other imaging methods. The dental practitioner also takes into consideration the patient preferences for a particular prosthetics, for instance, some patients may like to have fixed or permanent crown and bridgework instead of having removable ones. Patient financial situation and the time available is also factored in since a patient may not have the financial capability of having a particular type of implant installed.
Coming up with an accurate dental implant plan to a great extent will have a positive impact on the success rate of the implant and the lifespan of the prosthetic device. When it comes to general considerations, planning for a dental implant focuses on some few factors that include the general health condition of the patient, the jaws and the shape, position and size of the jaw bones, opposite and adjacent teeth and the condition of the mucous membrane. There are some conditions that a patient may be suffering from that deters him or her from being a candidate, and there are some that increase the risk of failure. People with poor oral hygiene, diabetic, and heavy smokers pose a great risk of getting a gum disease that may affect the implants. Also, people who have for a long time been using steroids and other disease may increase the chances of early dental implant failure.
During the planning stage, the dentist evaluates the health of the teeth. It is important that before a dental implant surgery is performed the teeth are healthy. Otherwise, there will be a great risk of failure. Some of the teeth health issues that the dental practitioner will look into include teeth decay, gingivitis, periodontal diseases and any other soft tissue conditions. The dental practitioner will also evaluate the presence of some chronic infections among other teeth health issues.
What Procedure is involved in A Dental Implant Treatment?
Placing the implant in most cases has five basic steps that include:
1. Soft Tissue Reflection
The first procedure is soft tissue reflection. In this process, the dentist first applies a local anesthesia to the patient and possibly sedation or general anesthetic. To access the jaw bone, the dentist will use a scalpel and score incisions in the overlying gum tissue that outline two separate flaps. The dentist will then use a hand instrument to push and peel each flap of gum tissue back so as to expose the gum tissue.
2. Creating the Pilot Hole

This process is where the dentist creates a pilot drill. A pilot drill is basically a small diameter drill bit that is used to create a hole which serves as a guide for other drills that will be used later on. The hole is made at high drill speed.
3. Completing the Pilot Hole
After making the pilot drill, the dentist will now extend the pilot hole to accommodate the full height and width of the implant. The measurement located on the drill helps the dentist to gauge this depth. This is done at low-speed drill. They use a water spray or a cooling saline to keep the temperatures down.
4. Placement of the Implant

At this step, the oral surgeon now places the implants screw. The implant screw can be self-tapping, but if it’s not, the prepared site is tapped using an implant analog. The oral surgeon then uses a torque controlled wrench to screw the implant into place. They use precise torque so that the surrounding bone cannot be overloaded. Overloaded bone can result in a condition known as osteonecrosis, which is a situation where the bone can die and may lead to failure of the implant, or it may not fully integrate with the jaw bone.
5. Tissue Adaption
After all the process above has been completed, the tissue is now left to adapt with the implant so as to provide a thick band of healthy tissue around the healing abutment. On the other hand, an implant can be buried where its top is sealed using a cover screw, and the tissue is closed to cover it entirely. After the implant has intergraded with the jaw bone, a second procedure will be done at a later date to uncover the implant.
Healing Time
For an implant to heal and become permanently stable, it needs to grow and completely fuse with the jaw bone through Osseointegration process. Tooth replacement cannot be done before the implant completely Osseointegrate with the jaw bone because if the dentist places it earlier, it may result in some movements that may eventually lead to implant failure. Due to this, a period of six months is allowed before a dentist can place a tooth on an implant. However, according to extensive research, the length of time an implant takes to heal largely depends on the initial stability of the implant rather than the length of healing time. As a result, the time that is allowed for an implant to heal largely depends on the density of bone implant placed and some other few factors rather than the uniform amount of time.
Additional Surgical Procedure
For an implant to completely fuse with the jaw bone through Osseointegration process, it needs to be surrounded by some healthy content of bones. Additionally, in order to survive on a long-term, the soft tissue (gingiva) around it needs to be healthy. It is a common occurrence for either the bone or the soft tissue to be deficient hence requiring the surgeon to reconstruct either before the surgery or after the implant placement.
Bone Grafting
The dentist will determine if the bone available in the jaw bone is sufficient for a dental implant through some methods like dental x-rays. However, today there are more advanced techniques that have been developed to judge the bone quantity in a jaw bone. There quite a number of factors that causes bone loss that includes: Whenever a tooth is lost or extracted, a considerable amount of bone that used to surround the tooth may disappear. The loss can be rapid within the first few months after losing a tooth. This process is referred to as bone resorption. As much as this process varies from individual to individual, there are some various measures that can be taken to reduce it. If there is poor bone grafting or bone loss continues after some time, a patient may start complaining that the implant is not as strong as it used to be in the long term.Bone can be harvested from various sources, but mostly it is harvested from the back of the teeth in lower jaw or the chin. Sometimes it can even extract from the thighs. The bone harvested from other parts is integrated and allowed to heal. During the healing process, the natural bone replaces the graft thus forming a new bone for the implant. For people who are suffering from a larger bone defect, there are some more invasive procedures that can be done on them. These procedures include mobilisation of alveolar nerve so as to allow permanent placement of fixture.
Soft Tissue (Gingiva) Reconstruction
Soft tissue reconstruction may be necessary to protect the teeth from the damaging effects of the gum recession. The procedure may also be undertaken just to improve the appearance of the patients smile. Gum recession is that process where the tissue that surrounds the teeth pulls away from the tooth, thus exposing more tooth. This brings damage to the supporting bone. Some methods that can be used to reconstruct soft tissue include connective tissue grafts. During this process, soft tissue is extracted from the roof of the mouth and tissue from the under the flap is known as sub epithelial, connective tissue is attached to the gum. The other method used is known as free gingival grafts. This method also involves removal of graft from the roof of the mouth, but now instead of getting the tissue from the under the flap, a small tissue is removed from under the mouth. The dentist may also use a method known as pedicle grafts. In this procedure, instead of getting tissue from the palate, tissue is extracted just from the area surrounding the tooth that needs reconstruction. This procedure is only done to people who have got plenty of gum near the tooth. At Carrum Downs Dental Clinic, dentists are specialised in performing bone grafting and soft tissue restoration in a way that it brings dental implant failure to zero
Maintenance
Proper maintenance needs to be provided to the implants after their placement. It is vital that the patient maintains good oral hygiene so as to increase the lifespan of the implants. Cleaning implants are not as hard. Actually, it is very similar to cleaning natural teeth. Restored dental implants should be kept free from plaque and clean twice a day through brushing and flossing. For most implant supported teeth, implants can be brushed and flossed just the way it’s done on natural teeth. It is especially important to clean implants immediately after every meal. This is done through brushing and giving attention to all sides of the implants.
Oral hygiene aids may include:
– Low-abrasive, tartar-control toothpaste
– Small, soft, electric or manual toothbrush
– Dental floss for cleaning around the abutments
Other supplies that the doctor recommends include
– Disclosing tablets to stain the location of plaque accumulation
– Antimicrobial mouth rinse
– Inter-dental brushes or any other aids that remove plaque between the teeth or either side of the implants
The patient must be committed not only to providing the dental implants daily hygiene at home but also to visiting the dentist on a regular basis. It is recommended that a dental implant patient should see a dentist after three to six months for professional cleaning and exam. Visit Carrum Downs Dental Group for a comprehensive dental check.
Risk and Complications
Dental implants surgery can be faced with some normal risks that include excessive bleeding, injury or damage to other teeth, infections and necrosis of the flap of the tissue around the implant. The atomic structures neighbouring the implants such as the maxillary sinus, blood vessels, and the inferior alveolar can be damaged as well in the process when the osteotomy is created or during the placement of the implant. Should a nerve be damaged in the process, the patient will experience numbness, lingering pain and tingling for an undetermined time. Additionally, there is the risk of inability to place the implant in the bone so that the implant can get stability can increase the risk of failure to Osseointegrate. While these risk may occur during a dental implant surgery, patients who chose reputable dental clinic to have the procedure performed like Carrum Downs Dental Group, the risk is reduced considerably. Check your dentist’s references and interview them thoroughly before making a decision that he or she is the best choice for you. Dentist at Carrum Downs Dental are well trained and have the necessary expertise to bring the risk of the dental implant to as low as zero.
Implant Failure
Uncontrolled diabetes, smoking, high alcohol consumption, untreated osteoporosis or high radiation exposure on the head or neck significantly increases the risk of dental implant failure. For women who are under postmenopausal, implant failure is more of a risk in the absence of the hormone therapy. Persistent infection at the surgical site, nerve impingement, loosening implant posts, lingual space or implant puncture of a sinus cavity is some of the causes of implants to be removed. However, if any of these problems can be corrected, a patient may become a good candidate for implants after the oral cavity is healthy.
Reduce Risk for Failure

There are many factors that increase the risk of failure of dental implants failure. Doctors and patients should work together to reduce the risk of failure by being thorough before, during and after the implant procedure. The patient should make a point of disclosing all the medical history to the dentist including medications. The patient and the doctor should be thorough during the planning stage and must commit to a thorough diagnostic. The doctor should also commit to using quality materials for the implant and the placement, low-quality materials and using shortcuts in the procedure may result in failure of the process. By spending the right amount of time and resources on a dental implant process, the chances of failure are significantly reduced.
At Carrum Downs Dental Group, dentists are very committed to walk every patient through the whole process and ensure that they brinTheg back that bright, beautiful smile and normal functioning of the teeth.